Bellevue: “America’s Most Storied Hospital” – An Interview with David Oshinsky

Bellevue Hospital Center provides high quality, respectful and accessible
health care services to the people of our neighboring community
and throughout New York City. Care is provided to all who require
clinical and social support regardless of ability to pay.
Bellevue Hospital
In the classic 1947 film Miracle on 34th Street, a kindly man named Kris Kringle is adjudged insane when he claims to be the real Santa Claus. He’s locked up for a time in a tiny cell at the notorious Bellevue Hospital on the East Side of New York City. Old Kris is eventually released and all ends well for him and the film’s romantic leads. But, thanks to such storylines about Bellevue in popular entertainment, many people imagine that the hospital is only a dumping ground for New York’s mental cases, a Bedlam in the Big Apple.
 In reality,
Bellevue today is a revered medical research facility associated with
New York University Medical School with a world-famous trauma center
and numerous twenty-first century specialized clinics as well as a
renowned psychiatric service.
In reality,
Bellevue today is a revered medical research facility associated with
New York University Medical School with a world-famous trauma center
and numerous twenty-first century specialized clinics as well as a
renowned psychiatric service.
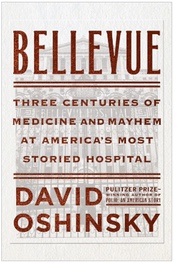
Award-winning historian Professor David Oshinsky explores the complicated history of this venerable public hospital from its humble eighteenth-century beginnings and through the aftermath of Superstorm Sandy and its recent Ebola patient in his groundbreaking new book Bellevue: Three Centuries of Medicine and Mayhem at America’s Most Storied Hospital (Doubleday). He writes, “The relentless focus on [Bellevue’s] eccentricities has obscured its role as our quintessential public hospital.”
As Professor Oshinsky stresses, Bellevue’s patients have come to the hospital for generations knowing they won’t be turned away regardless of their ability to pay. Bellevue has served as a safety net for the vulnerable and the marginalized: the poor, the mentally ill, immigrants, derelicts, the contagious, and others who were often refused treatment at other hospitals. Today more than one hundred languages are translated at Bellevue Hospital Center, a 25-story edifice where more than 600,000 patients are cared for annually in its emergency center and clinics.
In Bellevue, Professor Oshinsky traces the rise of the internationally-recognized hospital of today from a decrepit almshouse and pesthouse in the 1730’s. As he describes the evolution of Bellevue, he also tells the checkered story of American medicine with setbacks and breakthroughs in the treatment of illness and injury in each era through U.S. history. Bellevue was often at the cutting edge of medical advances as it created the first department of psychiatry, the first nursing school, the first medical photography unit, the first civilian ambulance corps, innovative life-saving medicines, therapies, and surgical procedures, and more.
Professor Oshinshy’s book is based on extensive research of archival records and other documents as well as dozens of interviews with physicians and others associated with the hospital. Critics have praised his exhaustive and original research as well as his lively prose and vivid storytelling.
David Oshinsky is a Professor of History at New York University, and Director of the Division of Medical Humanities at NYU Langone Medical Center. His other books include A Conspiracy So Immense: The World of Joe McCarthy, winner of the Hardeman Prize for the best book on the U.S. Congress; Worse Than Slavery, winner of the Robert F. Kennedy Prize for distinguished contribution to human rights; and Polio: An American Story, winner of the Pulitzer Prize in History and the Hoover Presidential Book Award. He is also the recipient of the Dean's Medal from the Bloomberg-Johns Hopkins School of Public Health for his distinguished contributions to that field.
Professor Oshinsky generously responded by email to a series of question on his work and his history of Bellevue.
Robin Lindley: You’ve written widely on history, Professor Oshinsky, with prize-winning books on McCarthyism, racism and Jim Crow, and more recently your Pulitzer Prize-winning history of polio, and now your history of Bellevue Hospital. How do you see your evolution as an historian since you began writing and teaching?
Professor David Oshinsky: My career path certainly has been unusual. I’ve moved from one field to the next, with no logical progression beyond my own curiosity.
I wrote my doctoral dissertation on an aspect of McCarthyism, followed by a full-scale biography of the Red-hunting senator. By that time, I had said pretty much what I wanted to say. Not everything of importance, of course—not even close. But I felt it was time to explore something new.
To be honest, I stumbled upon my next book project—race and punishment in the post-Civil War South—quite by accident. My good friend Steve Whitfield, the distinguished Brandeis University historian, was heading down to Mississippi to do a book on Emmet Till, and I tagged along. Steve went to the Delta, where the Till murder had occurred, while I went to visit the State History Archives in Jackson. Looking for I topic, I spoke to an archivist who guided me to material on Parchman Farm, the legendary prison-plantation, which included the pardon files spanning more than a century. Each file was akin to a social history of a prisoner, allowing me to recreate both the lives of these people and workings of a racial order in which punishment and incarceration played a dominant role. The material was so rich that I just stood aside and let the story tell itself
I never pretended to be a Southern historian, though Worse Than Slavery remains, in many ways, my favorite book. After its publication, I moved in yet another direction.
I’m a product of the baby-boom era, and among my most vivid memories is the scourge of polio, which descended each summer like a plague, crippling and killing thousands of children. Polio is a very visual disease—kids in leg braces and wheel chairs, iron lungs lined wall-to-wall in hospital wards. Beaches and swimming pools closed. Kids were kept out of movie theaters and bowling alleys. My parents rented a bungalow in the mountains every summer, just to get us away from the “polio germs” in New York City.
I decided to write a social history of the disease, from the intense public anxiety to the bitter scientific race for a protective vaccine. What most interested me, though, were the revolutions in philanthropy and medical research spurred by the polio crusade in the era before serious federal involvement and the growth of “Big Pharma.” Everything from the massive fund-raising to the vital scientific breakthroughs to the largest public health experiment in American history sprang from a culture of public voluntarism, unlikely to be repeated today.
Polio: An American Story was published in 2005. The timing was perfect. It coincided not only with the 50th Anniversary of the Salk Polio Vaccine, but also with the resurgence of an anti-vaccine movement based largely upon misinformation and fake science.
The idea of remaining in the field of medical history, where my voice might make a small difference, held a strong appeal.
Robin Lindley: What inspired your new book on New York’s Bellevue Hospital?
Professor David Oshinsky: Again, as a New Yorker born and bred, the reputation of Bellevue was something I couldn’t escape. I knew what I (and millions of others) got from movies such as Lost Weekend, Miracle on 34th Street, and The Godfather, from TV shows like Law and Order, and from the endless list of “celebrities” who passed through its massive psychiatric wards, from Allen Ginsberg to Norman Mailer to John Lennon’s assassin, Mark David Chapman. The phrase, “Taken to Bellevue,” was a national punch line.
I returned to New York City in 2012 to join the History Department at NYU and to design a Medical Humanities Program at NYU Medical School. Having spent twelve glorious years at the University of Texas at Austin, the decision wasn’t easy. But among the lures was the chance to write about Bellevue, NYU’s largest teaching hospital, where, as luck would have it, my medical school office is located. I quickly immersed myself in Bellevue’s storied history, stretching back three centuries. The media’s description—a receptacle for mangled crime victims, lunatics, and derelicts—wasn’t entirely incorrect. I prefer to call it incomplete—one part of a complicated story.
Robin Lindley: Relating the history of an institution must be a different problem for a historian than writing a history of an event or person. What was your strategy for Bellevue?
Professor David Oshinsky: What I’ve always tried to do, regardless of the subject, is find interesting characters to drive the narrative, each one helping to focus the reader on a thread of the larger story I hope to tell.
This book was more challenging because there are numerous story lines: immigration, public health, epidemics, and medical progress told against the background of an evolving city— America’s largest and the world’s most diverse. To compound matters, much of Bellevue’s archive was wiped out in Superstorm Sandy.
Fortunately, there is a wealth of material about Bellevue at the New York Historical Society, the New York Academy of Medicine, the Municipal Archives, and paper collections scattered throughout the country. I also interviewed scores of longtime Bellevue folks, some with private papers to share.
Robin Lindley: What surprised you the most in your exploration of Bellevue?
Professor David Oshinsky: Two things, really. First, that Bellevue is so much more than a “mental institution,” though its psychiatric wards do take up several floors of the main patient tower. When a cop is shot in Manhattan, a firefighter is overcome with smoke, a construction worker falls from a scaffold, Bellevue is the destination. Should the pope or the president take sick in New York City, Bellevue awaits. What other hospital has two massive prison wards, with a full courtroom ready for use? Or a sealed ward for drug resistant TB patients? Or a special clinic for the worldwide victims of political torture? Doctors and nurses report cases of a foreigner arriving at Kennedy Airport, hailing a cab, and uttering a single word: “Bellevue.”
Second, that Bellevue always attracted the best clinicians and researchers. The place is a magnet. From the outset, doctors saw Bellevue as a moral or religious calling. They came because they knew they would see every imaginable affliction known to humankind. And some were attracted, quite frankly, by the chance to experiment on what I call “uncomplaining bodies”— charity cases lacking the power to say no.
The ledger of those who trained and worked at Bellevue reads like a “Who’s Who” of American medicine: William Welch, the father of American pathology; Valentine Mott and William Halsted, the most brilliant surgeons of their time; Walter Reed and William Gorgas, who tamed Yellow Fever; Albert Sabin and Jonas Salk, who developed the two polio vaccines; Andre Cournand and Dickinson Richards, who perfected cardiac catheterization.
Robin Lindley: What else makes Bellevue special?
Professor David Oshinsky: Foremost, I think, is its longstanding relationship with several of the nation’s top medical schools. From the outset, Bellevue was serviced by the College of Physicians & Surgeons (Columbia); then by the new NYU Medical College in the 1840s; followed by Cornell Medical School in the 1890s. Indeed, Bellevue even created its own medical college in 1861, which eventually became part of NYU.
By 1900, Columbia, NYU, and Cornell had their own separate medical and surgical divisions at Bellevue, servicing the patients in return for training their students, residents, and attending physicians.
Today, only NYU remains. It receives close to $170 million annually from the city to meet the hospital’s medical needs.
What this means is that Bellevue has always been at the center of medical education and scientific discovery.

The revered Bellevue Hospital grew
from an alms house built in 1736.
Robin Lindley: How did Bellevue get its name and when did it open?
Professor David Oshinsky: Its origins are remarkably mundane. In the 1790s, the nation’s eastern port cities were devastated by a series of Yellow Fever epidemics. New York City had so many deaths that iconic Washington Square, in the heart of today’s Greenwich Village, was used as a mass burial ground for epidemic victims. Searching for a place to quarantine the sick, the city chose an old estate on the East River known as “Bell-Vue.”
What struck me was the heroic dedication of the young physician hired to run this “pest house.” His name was Alexander Anderson. He was twenty-three years old. He had come to Bellevue because he believed it to be his Christian duty to help the sick. And the personal suffering he faced once there was unimaginable. In the Epidemic of 1798, he lost his only child to Yellow Fever, then his wife, both parents, and a brother. Yet he remained at Bellevue almost to the end, comforting the survivors.
When epidemic disease struck New York City—cholera in the 1830s, typhus in the 1840s and 50s, tuberculosis in the late 19th century, influenza in 1918-1919, AIDS in the 1980s— Bellevue played its appointed role.
It’s no surprise that New York City’s lone Ebola patient in 2014 wound up on the very ground where Alexander Anderson began his medical career.
Robin Lindley: What role did Bellevue play during the Civil War?
Professor David Oshinsky: Bellevue treated hundreds of wounded Union soldiers returning from the field. After Gettysburg, its wards overflowed. Yet, since many of Bellevue’s surgeons had already enlisted, the care was often handled by inexperienced contract doctors hired by the army.
More controversial, however, was the medical treatment received by injured anti-draft rioters who tore New York City apart in 1863. They flooded the hospital, barely separated from the Gettysburg returnees. As always, no one was turned away.
Robin Lindley: How did Bellevue push hospital innovation in this era?
Professor David Oshinsky: As the nation’s largest hospital by 1870, Bellevue took the lead in clinical practice and medical research. It opened the nation’s first maternity ward and the first nursing school for women, the first civilian ambulance service and the first department of medical photography. It offered the first courses in pathology for medical students, and became a leader in neurology, bacteriology, pediatrics, and orthopedic surgery. Its physicians, including Stephen Smith, helped turn the concept of public health from a well-meaning cause into a highly trained profession. And its laboratories gave birth to the field of forensic medicine, with New York City’s fabled Medical Examiner’s Office just a stone’s throw away.
Robin Lindley: Isn’t it true that Bellevue doctors in the latter half of the nineteenth century treated four American presidents?
Professor David Oshinsky: Yes—for better and worse.
In April 1865, a young army surgeon named Charles Augustus Leale, recently graduated from Bellevue Hospital Medical College, was the attending the play, “Our American Cousin,” at Ford’s Theatre when he heard a gunshot and saw John Wilkes Booth jump to the stage. A call went up for a doctor, and Leale rushed to Lincoln’s box. As the first physician on the scene, Leale did all he could do to aid the mortally wounded president. Leale’s role in this episode, as I explain in the book, is a lot more complicated than is generally known, though Leale did perform well under unimaginably difficult circumstances. Unfortunately, his version of what actually happened that tragic evening changed dramatically over time.
In the 1880s, former President Grant’s personal physician, Bellevue’s Fordyce Barker, offered the correct diagnosis of inoperable throat cancer.
And when President Garfield was shot by an assassin in Washington’s main railroad depot in 1881, Bellevue’s distinguished military surgeon, Frank Hamilton, was called to the White House for consultation. We know today that if Garfield had simply been left alone, he would have survived. Neither of the two bullet wounds was remotely fatal.
But Frank Hamilton was “old school.” He didn’t believe in antiseptic medicine or germ theory. He thought Joseph Lister and Louis Pasteur were pompous frauds, spreading false theories about invisible organisms that didn’t actually exist. The fact that 50 percent of Bellevue’s patient amputees died of post-operative infection within a month of their operations seemed, to Hamilton, to be the natural order of things. He didn’t see the point in washing his hands or sterilizing his instruments. And he wasn’t alone.
Hamilton examined Garfield by sticking unwashed fingers and dirty probes into the president’s wounds. The result was inevitable. Garfield soon was ravaged by infection. Hamilton stayed by Garfield’s side in the two months between the shooting and the president’s death, issuing optimistic bulletins to an increasingly anxious public. Meanwhile, Garfield wasted away, his autopsy showing the massive, pus-filled, pockets of infection. The good news was that Garfield’s death triggered a public debate about the need for antiseptic procedures in hospitals—not to mention the overdue acceptance of germ theory.
The story doesn’t end here. Twelve years later, Bellevue physician Joseph Bryant, President Grover Cleveland’s personal physician, noticed a mass in Cleveland’s mouth. When it turned out to be cancerous, Cleveland demanded a secret operation to remove it, fearing that the news of his illness would embolden his critics. Bryant then assembled a team of Bellevue doctors, using a specially fitted yacht as an operating room. Sailing up the East River, and passing Bellevue with the shades drawn, the yacht made its way to a calm part of Long Island Sound, where the mass was removed using every antiseptic precaution— starched gowns, boiled instruments, disinfected quarters, and the like.
Cleveland would die of a heart attack fifteen years later, his life extended, in no small part, by the bitter legacy of President Garfield.
Robin Lindley: What was the treatment of women and minority doctors like at Bellevue in these years?
Professor David Oshinsky: Not good—and not especially surprising—though Bellevue’s record was better than most.
Relying on the three medical schools—Columbia, Cornell, and NYU—to supply the house staff and attending physicians, Bellevue had almost no female doctors until the early 20th Century, when these medical schools began admitting women in small numbers. Most went into pediatrics and obstetrics, where women, seen as nurturers, were more readily accepted.
World War 1 also broadened opportunities for women, because so many male doctors were drafted, creating a shortage of physicians. At Bellevue, women like Edith Lincoln, who organized the hospital’s pediatric tuberculosis service, and Lauretta Bender, who ran the children’s psychiatric wards, became leaders in their fields.
Bellevue saw very few African-American doctors until the 1970s, and the numbers, even today, remains depressingly low—a problem still plaguing medical schools and hospitals throughout the country.
The major breakthrough at Bellevue in these years occurred with Jewish doctors. Cornell and Columbia had rigid “Jewish quotas” well into the 1950s, as did every major medical school on the East Coast, with one notable exception: NYU accepted Jewish applicants without prejudice. And since NYU ran the largest of the three divisions at Bellevue, the hospital became a sanctuary for Jewish physicians.
Robin Lindley: What are some of the major developments that have marked Bellevue in the modern era?
Professor David Oshinsky: Bellevue is a microcosm of New York City. It’s always been that way. One can chart the severity of a New York winter by counting the flu and pneumonia victims on the hospital’s chest service. When AIDS arrived in the 1980s, when violent crime spiked, when addicts turned to crack cocaine, when homelessness became epidemic, Bellevue usually saw it first.
The story of AIDS at Bellevue is complicated. More AIDS patients were treated there, and died there, than at any hospital in the country. It’s not an unbroken narrative of heroism. Doctors, nurses, and staffers were panicked by the disease. Some refused to do their jobs early on, not knowing how to protect themselves from a disease that killed all its victims. It took time—and a lot of training and reinforcement—to get everybody on board. And the emotional toll it took on the younger physicians in particular, unable to stop the suffering of people their own age, was profound.
Still, Bellevue admitted hundreds of AIDS patients at a time when many neighboring hospitals were doing just the reverse. I often ask my students to see Larry Kramer’s riveting play—now an HBO movie—The Normal Heart, to get a good sense of the bravery and compassion shown at Bellevue during the decade-long AIDS epidemic. And my book covers the development and testing of the multi-drug cocktail that helped turn AIDS from a death sentence into manageable condition.
In the mid-1980s, as crime and homelessness soared in New York, the city turned one of Bellevue’s abandoned psychiatric buildings into a men’s shelter. Before long, the homeless were using Bellevue’s public spaces as an extension of that shelter—using the lobbies and bathrooms, stealing food from patients’ plates, and even squatting in poorly patrolled parts of the hospital. In 1989, a deranged homeless man raped and murdered a pregnant Bellevue pathologist in her office. For many, the incident was an accident waiting to happen, and a heated debate began over both the inadequate security and the limits to Bellevue’s ethos of compassionate care. Was Bellevue a hospital or a bus station waiting room? The answer, as I attempt to demonstrate, did not come quickly or easily.
More recent events—from 9/11 to Superstorm Sandy in 2012—showed Bellevue’s enormous resilience. The storm devastated the hospital, forcing it to close for the first and only time in its history. Holding out for 48 hours on back-up emergency power without air conditioning and running water, the hospital evacuated its 700 patients in semi-darkness: prisoners, psychiatric patients, infants and the elderly, infectious TB patients—everyone got out safely. Following massive repairs, Bellevue fully reopened a few months later.
Robin Lindley: What does the future hold for Bellevue?
Professor David Oshinsky: Public hospitals are in trouble. In the past three decades, they’ve been closing in droves. Even in New York City, which guarantees free care to the indigent sick, the number of public hospitals is rapidly declining. Understaffed and underfunded, they still are expensive to run because so many of their patients are undocumented, or uninsured, or both, with multiple medical issues and no access to primary care beyond an emergency room.
As a so-called safety net hospital, serving the underserved, Bellevue relies on the state-funded Indigent Care Pool and the federal government’s Disproportionate Share Hospital plan to subsidize what the city can’t afford to pay. But these subsidies are declining, and Obamacare’s restrictions on undocumented immigrants, who are ineligible for public coverage, make things that much harder.
Still, Bellevue is a survivor. Its ionic history, unparalleled emergency services, and quality medical care, give it a special edge. Bellevue remains the grand dame of America’s public hospitals, and it’s impossible to imagine New York City without it.