A History of Huntington Disease and Beyond
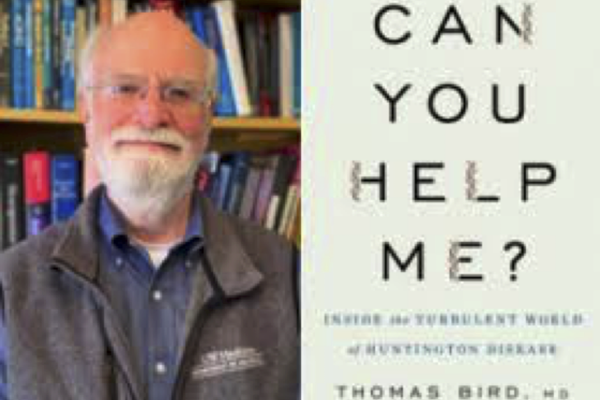
In 1974, young neurologist Dr. Thomas Bird founded the first clinic for adults with neurogenetic diseases in the United States. For more than 40 years, he directed this clinic at the University of Washington where he saw thousands of patients and conducted pioneering research on conditions such as cerebellar ataxia, movement disorders, hereditary neuropathy, muscular dystrophies, and familial dementias. Over his career, he has been honored with numerous national awards and lauded for his discoveries about the genetics of hereditary neurological disorders including Alzheimer and Huntington diseases.
To his initial surprise, patients with the cruel and incurable Huntington disease became a prominent part of Dr. Bird’s practice in the early years of his clinic. Huntington’s is a progressive, inherited disease that perniciously and ruthlessly devastates the brain. It can cause incoordination, jerkiness, confusion, impaired judgment, emotional instability, depression, anxiety, social disinhibition, hallucinations, and other problems. And no two patients are alike in terms of their signs and symptoms of the disorder.
Dr. Bird addresses this perplexing disease and its many permutations in his groundbreaking new book for general readers and professionals alike, Can You Help Me?: Inside the Turbulent World of Huntington Disease (Oxford University Press). The title comes from a Huntington sufferer’s plea for help from his prison cell, and this desperate call reflects the desire of so many of Dr. Bird’s patients who, through the years, sought his unique understanding and care.
In his book, Dr. Bird vividly describes Huntington disease, traces its history and, at the heart of his book, shares dozens of accounts of his own patients in lively prose that evokes the engaging writing of renowned doctor-authors such as Oliver Sacks, Richard Selzer and Atul Gawande. He recounts the physical, cognitive and emotional challenges of his patients and the complex situations that patients and their families face every day. There are wrenching stories of neglect and abuse of vulnerable Huntington sufferers as well as stories of hope and courage and the unselfish—and vital—support of families and friends. These very human accounts come from Dr. Bird’s decades of meeting and treating Huntington patients of all ages, from early childhood to the nineties, and from all walks of life.
Physicians are still struggling to understand the clinical manifestations of this condition. No Huntington’s patient is “typical,” as Dr. Bird’s case studies demonstrate. One patient may exhibit jerky movements only, while another may be emotionally explosive with poor judgment but without an obvious movement disorder. Some may experience both severe physical and behavioral problems, especially as brain degeneration progresses. Some patients may alienate their caregivers and some may refuse care and some may lack the financial and other resources to receive care and to survive in today’s complex world.
Can You Help Me? reflects Dr. Bird’s compassion and care for patients of this dreaded disease as he offers support and treatment grounded on his trailblazing research into the genetics of neurological diseases. In offering understanding and empathy to each patient, he emulates the admonition of the legendary physician Sir William Osler: “Care more for the individual patient than the special features of the disease.”
Dr. Bird is a University of Washington Professor (Emeritus) of Neurology and Medicine (Medical Genetics). In addition to directing the UW Neurogenetics Clinic for more than 40 years, he was also chief of neurology at the Seattle VA Medical Center for 12 years and is presently a retired Research Neurologist in Geriatrics at the VA.
Although retired from clinical practice, Dr. Bird still actively researches genetic diseases of the brain and neuromuscular system; collaborates with molecular biologists and others on genetics projects; and mentors physicians in training and research fellows. He earned his M.D. from Cornell Medical College and is board certified by the American Board of Psychiatry and Neurology. He lives in Lake Forest Park, WA, just outside Seattle, with his wife Ros.
Dr. Bird sat down at his University of Washington Medical Center office and generously responded to questions about his career and the history and human stories of Huntington disease.
Robin Lindley: Thank you Dr. Bird for talking with me about your distinguished career and your new book on Huntington disease. I’d like to first ask you about your own story. When you were a child, did you dream of becoming a doctor?
Dr. Thomas Bird: I grew up in a small town in upstate western New York, in the Finger Lakes area. My maternal grandfather was a country doctor in that small town. I didn't know him really. He died when I was five or six years old, so I only have a few vague memories of him. But our house where I grew up was just down the street from where he lived, and that was the family home on my mother's side, and my mother's brother, my uncle lived in that house, so I was very familiar with the house.
My aunt and uncle kept my grandfather’s old office intact. I remember wandering through it as a kid and seeing the examination chair and a little side laboratory with a microscope and shelves loaded with pill bottles. I was very impressed.
So, I had this knowledge of my grandfather, even though I didn't know him. My mother clearly adored him so, when I was growing up as a kid, it was very clear to me that if you wanted to be the best you could be, you would become a doctor. That was never said explicitly, but it was the aura that I grew up with. Later I got really interested in chemistry and thought I wanted to be a chemist. So it wasn't like I directly wanted to be a doctor. But when I went to college, it was certainly in the back of my mind because I became a premed major.
Robin Lindley: What inspired you to specialize in neurology?
Dr. Thomas Bird: There were a lot of lines that led to that. I'm sure that having a brother with mental retardation made a difference in how I viewed people and how I viewed medicine and the things I was interested in. Having a brother that I lived with 24/7 my whole childhood life who had something not right with his brain impacted me a lot. And, when I went to college at Dartmouth, I actually majored in psychology and who knows exactly all the influences for why I did that, but my brother was probably part of it.
I also was just fascinated by human behavior. Fortunately for my future, the psychology department specialized in biological psychology so the faculty were very interested in the neuroscience brain piece of psychology. We had Skinner boxes where we did mouse and rat and pigeon experiments on behavior, and I took one course where we dissected a sheep brain and then a human brain. I think that made a difference. My mentor was a clinical psychologist who was actually in the department of psychiatry at the medical school as well as in the department of psychology. He taught me a lot about human behavior and our interests in that topic matched nicely.
So, when I went to medical school, I thought my trajectory would be to either be a family doctor, like my grandfather, or a psychiatrist because I was really interested in human behavior. When I got there, I didn't particularly like psychiatry. It wasn't a neuroscience or brain-oriented department of psychiatry so I lost interest in it.
Then, mostly by chance, I ended up having my summer project with the new chairman of the department of neurology at Cornell, Fred Plum. I knew nothing about neurology, but I wanted to stay on campus and work with somebody doing research in medicine. So I got hooked up with Dr Plum. He turned out to be a very dynamic, aggressive, energetic person who eventually became world famous. He wrote a bestselling textbook in the 1960s called Stupor and Coma, and he became one of America's leading neurologists. In the beginning I had no idea who he was or what I was getting into, but it turned out to be terrific.
I started with a clinical project in coma. I learned how to do EEGs [electroencephalograms], and I was going around the hospital with a mobile EEG machine and doing EEGs on people in comas. So I got to see all kinds of neurology and I got to see it up close and personal. Then I started going to neurology grand rounds on a regular basis. I just became fascinated with the brain and with neurology.
Back in those days, you didn't have to decide what you wanted to specialize in until you got into your internship. My internship was here at the University of Washington, and I already knew I was interested in neurology. In my internship, I had two neurology rotations and I just loved it and had a great time. The head of neurology department asked me if I’d like to be in the neurology program? And I said, "Sure." And that was it. That was before the days of matching for residency programs and before the days of signing a contract. It was just on a handshake.
Robin Lindley: And you then further specialized in genetics and neurology.
Dr. Thomas Bird: So I was in neurology, which I really loved. Then, in my last year of the neurology residency, I learned of the Medical Genetics Clinic here that had been started by Arno Motulsky who was one of the very earliest and most prominent medical geneticists in the country. He started medical genetics here at the University of Washington in 1957 and, along with Johns Hopkins, that was the first program in the country looking at the genetics of human disease with a medical orientation. He was very farsighted in doing that initiated a clinic that saw adults with genetic diseases.
So, as a senior neurology resident, I started going to that Medical Genetics Clinic and seeing the kinds of patients that I'd never seen before. They were all considered rare diseases--back of the textbook experiences. I'd go to my general neurology clinic and I'd see migraines and back pain and stroke and things like that, which were kind of interesting but I didn't consider them fascinating. And I'd go to this genetics clinic and I'd see Huntington's disease and cerebellar ataxia, muscular dystrophy, and Charcot-Marie-Tooth neuropathy. Things I'd never seen before. And I was fascinated by it. I discovered they had a fellowship training program associated with the clinic. I applied for the fellowship and was able to get some funding.
After I finished my residency, I did two years of fellowship in medical genetics and that became my career. I spent the rest of my career specializing in genetic diseases of the nervous system. Nobody did that back then for adults. It was a new area and it turned out to be very timely. I didn't realize it, but I was right on the cutting edge of a revolution in human genetics.
Robin Lindley: I'm very impressed by your extensive background. You're a pioneer in the medical genetics of neurological diseases, including Huntington disease, the focus of your new book, Can You Help Me?
Dr. Thomas Bird: I started a clinic in adult neurogenetics as a fellow in 1974, 45 years ago. At that time, in the 1970s in 1980s, the most common neurological disease seen in the medical genetics clinic was Huntington's disease. I had no idea that was the case until I got to that clinic. It was considered a rare disease, and yet there were people coming in with it every week. Because it was so common in that clinic, it became something that I couldn't avoid. And I found it extremely fascinating. So I saw what eventually developed to be hundreds of families with Huntington's disease over the next several decades.
Robin Lindley: I realize it's complicated, but what is Huntington disease or Huntington's chorea, as it was once called?
Dr. Thomas Bird: It was called Huntington's chorea for a long time. In a nutshell, it's a degenerative disease of the brain that's genetic. Those are the key things to know. So it's a brain disease. It's degenerative, so it's progressive and causes a deterioration in the brain. And it's inherited in what's called a dominant fashion. So, if someone has it, each of their children has a 50/50 chance of inheriting it whether they're a boy or a girl, and that's each time they have a child. And it's so progressive that it eventually is fatal. But it's slow, so the typical duration of the disease is about 15 years.
The manifestations of the disease primarily fall into three categories. One is trouble with their coordination and [patients] develop movements that they can't control. They have these jumpy, jerky, uncoordinated movements, and it can affect the hands, or the arms, or the legs, or the face. It can affect their whole body. So they develop these jumpy, jerky movements, and when they're walking, they almost look like they're dancing in an uncoordinated way. And that's why it got called chorea. Chorea is the Greek root word for dance, as in choreography, and chorea means dancing. And these people sometimes look like they're doing a dance.
Second, they also can develop a kind of dementia. So their judgment and their ability to solve problems can become mildly to moderately to severely impaired.
And third, they can have problems with behavior with disinhibition where they're unable to inhibit socially inappropriate activity. And their thinking can become disoriented or disarranged. They can become manic or they can become depressed or they can have delusions or even hallucinations. Their behavior can become quite abnormal.
Any of those things can happen to a person with the disease. And someone can just have mostly one symptom or a combination of two or all three. The dramatic piece that people notice is the chorea, and that's why it was called Huntington's chorea. But it became clear to doctors and investigators that there were people who had the disease with little or no chorea and, to be more comprehensive in terms of the name, it was called Huntington's disease rather than Huntington's chorea because Huntington's chorea implied that everybody had chorea and not everybody with it has chorea.
Robin Lindley: How common is Huntington's? It's thought of as very rare.
Dr. Thomas Bird: Everything is relative. It is rare. If you relate it to Alzheimer's or Parkinson's or cancer or diabetes, it's much more rare than those diseases. It's on the order of 10 cases per hundred thousand population. So that's not a lot, but it's actually more common than ALS (amyotrophic later sclerosis) or Lou Gehrig's disease, which people have heard a lot about. And it's more common than some other genetic diseases. So, it's not common, but it's not as rare as you might think.
We've seen hundreds and hundreds of families in Seattle. In my career, I know I've seen more than a thousand people with the disease. I don't think of it as rare. I think of it is uncommon, which is somewhere between rare and common if that makes sense.
Robin Lindley: There is no cure for Huntington disease and it's fatal.
Dr. Thomas Bird: Right. So a couple of things to put it in context. First of all, it's called a fatal disease because people with it have a shortened lifespan and they get worse, then they die with the disease, usually of the things that happen to people who can't take care of themselves. It's the same as what happens when you get end stage Alzheimer's or end stage Parkinson's or end stage ALS. It's not really the disease that kills you, but you can't walk, you can't talk, you can't swallow, and you develop malnutrition and pneumonia and that's what you die of. But there's no question that lifespan is shortened, and that's why it's called a fatal disease.
But I always remember a woman who is very famous in the world of Huntington's disease. Her name was Marjorie Guthrie. She was Woody Guthrie's wife. When people said, this is a fatal disease, she would get a little upset about that word fatal. She would look you in the eye and say “life is a fatal disease” because she didn't like HD being labeled that way. She said everybody dies of something sooner or later so let's not get too down about this disease. Let’s be more optimistic and move forward.
And there is not a cure for this disease. What does that mean? That means that once it starts, there's nothing that stops its progression and there's nothing that prevents it from developing, and people continually go downhill with it. So, in that respect, there is no cure.
Robin Lindley: As you detail in your book, genetic testing is available for Huntington’s. Understandably, people who are aware of ancestors with the disease are often reluctant undergo testing.
Dr. Thomas Bird: In 1993 medical science developed the ability to have a simple blood test to identify the mutation causing HD. That dramatically changed the field. Now people at risk for the disease could actually find out if they had or had not inherited the HD mutation. Obviously that testing decision is fraught with all sorts of complications. Because there is no effective treatment, most people decide not to be tested. Those that do get tested may experience the gamut of emotional reactions from elation to serious depression. In my book I have an entire chapter devoted to this amazing and often unpredictable range of responses.
Robin Lindley: In looking at the history of the disease, Woody Guthrie is perhaps the most well-known Huntington disease sufferer. He’s an example of a patient. What do we know about his disease course?
Dr. Thomas Bird: We know a lot about him for many reasons. One, he was famous so a lot was known about him and he wrote his own autobiography. I've tried to read that. I haven't read it cover to cover. It's a strange story. In the first hundred pages, he goes into great detail about growing up as a kid in Oklahoma. And he talks about his friends and he talks about the games they played, and about the town he grew up in, and about the tricks that they played. He talks about the trouble they got into and he goes on and on about those things.
Of course, he didn't know that his mother had Huntington's disease. But once you get into his book, he talks about his mother and how he loved her. And he didn't understand why she would behave the way she behaved. She would lose her temper and she would scream and yell and she would throw dishes and she would run out of the house. And she was clumsy and she was always breaking things. He had no idea why, and he loved her dearly, but he recognized that there was something wrong with her.
And so, you learn that as his background, and then he became this famous folksinger who was highly popular. Then he began to develop the disease and his behavior changed and his thinking changed and he developed chorea. It became obvious that he had the same disease that his mother had. He got the diagnosis of Huntington's chorea and he eventually was institutionalized. He died in a state institution.
Robin Lindley: You detail the history of Huntington disease, which was not identified until the late 19th century, although it certainly had affected humans for thousands of years.
Dr. Thomas Bird: Yes. It's called Huntington's because that's the name of the young doctor that first described it best. In terms of history, it's a fascinating story. George Huntington, who the disease is named for, grew up in a little country village, East Hampton, Long Island, in the middle of the 19th century. His father and his grandfather were family doctors in that town. He went around with his father on rounds to see patients. He described going with his father in a buggy, and riding to the homes of people who had this disease. There was a family of people that had chorea and it ran in their family, so he knew about them as a kid because he had seen them with his father. He had grown up knowing of the characteristics of this family.
Then Huntington went to medical school, just like his father and grandfather, and became a family doctor. After medical school in New York City, he briefly moved to Ohio to try out a practice. While he was there, the local medical society asked him to present a paper. That was a professional organization and probably every week or every month they had one of their members present a paper. They asked him to do it as a new member. He presented a paper on chorea and I think it's partly because he knew this family, so it was something he felt comfortable writing about.
So, he presented this paper on chorea to the local county medical society and it was so good, he wrote it up and published it. He talked about all different kinds of brain diseases that can produce chorea. At the end, almost as an afterthought, he said he'd like to mention this family he’d known for decades in his hometown because they're so interesting. Then he goes through a very accurate, careful description of the family in terms of their movements, their behavior, their loss of judgment and dementia. He described the fact that the disease was progressive and fatal. The fact that they had an increased frequency of suicide. The fact that males and females both got it. The fact that it was passed down from generation to generation. And if somebody had a parent with it, but that child lived into late adulthood and never showed signs of it, then it didn't show up in their branch of the family. So, Huntington really had cued into the genetic piece of it before medical genetics, and [before geneticists] knew about dominance. He had described dominant inheritance and he didn't even know what he was describing.
He published this paper about chorea in 1872 when he was just 22 years old. Over the next 20 to 30 years, other people in the US and in Europe realized they were seeing similar families. And they would write them up. And when they referred to them, they would always say we've seen a family with chorea and it's like this family that Huntington described and they would cite his paper. And so very quickly it got to be called Huntington's chorea because he was the one that first described it. And that was an 1872.
Robin Lindley: In discussing medicine and genetics, you mention a resurgence of interest in Gregor Mendel’s work in genetics a couple of decades later.
Dr. Thomas Bird: Yes. In 1900, biomedicine rediscovered Gregor Mendel's laws of inheritance. Mendel, the monk with his pea plants in what's now the Czech Republic, figured out inheritance of genes. Genes weren't actually known at the time, but that's what Mendel was studying. He found out that things could be inherited in a dominant or recessive manner. And he very accurately and carefully described that and it was pushed aside and unrecognized and nobody thought anything about it for 30 years. And then in 1900, his papers were rediscovered, and people not only realized that it was relevant to the plant world, but they said, "Oh my goodness. Human diseases are inherited in the same way."
A scientist named Bateson in England was looking around for human diseases that he could say were dominant or recessive, like Mendel's pea plants. He came across the publications on Huntington's chorea and he looked at the pedigrees of families with Huntington's chorea and said, "Oh my goodness. This is autosomal dominant inheritance." This is what Mendel was describing in his pea plants as dominant inheritance occurring in the same way in a human disease. Bateson started promoting that idea and Huntington's chorea suddenly moved to the front of the book in human genetic studies because it was considered a classic example of dominant inheritance. Even though it was rare, it became very well known in the human genetics field because it was very clear that it was an autosomal dominant disease.
Robin Lindley: Was Parkinson's disease described by then too?
Dr. Thomas Bird: Parkinson's definitely was already described, but nobody thought it was genetic, so it wasn't part of the human genetics literature at all. Same with Alzheimer's. Alzheimer's was described about 1906 or 1907, and was a well-recognized disease, but no one really thought it was genetic. But Huntington's was special because it was clearly a genetic.
Robin Lindley: How this whole field has developed is fascinating. And the gene for Huntington’s wasn't identified until about 1993?
Dr. Thomas Bird: Yes, the gene was found in 1993.
Robin Lindley: It's incredible that Huntington was so far sighted.
Dr. Thomas Bird: The key advantage he had was realizing [the disease] was genetic, realizing that it was inherited. And he knew that because he had lived in the context of his family and his community for his whole life. He had seen several generations of this family and had no doubt it was inherited. As I mentioned he described the disease when he was 22 years old and never wrote another paper. He wasn't an academician at all. He never did research.
Robin Lindley: Huntington was more of a country doctor then?
Dr. Thomas Bird: He wanted to be a country doctor and he was a country doctor.
Then a couple of things happened with Huntington's that are of historical interest. One, a psychiatrist, I believe in Connecticut, saw families with this disease. He thought that the families in New England that had this disease were all related to each other, and that they had come over as migrants from England in the 1600s. And he thought he had evidence that they were persecuted as witches in New England in the 1600s and 1700s. He wrote about that, and that became a very popular theme about Huntington's disease that made people very uneasy.
Robin Lindley: Did this psychiatrist connect his view of Huntington’s with the Salem witch trials?
Dr. Thomas Bird: He thought so, but he wasn't able to quite make that connection. But it turns out he was wrong. He was wrong that they were all related to each other. He was wrong that they came over at the same time. And, as far as anybody can tell, he was wrong about them being persecuted as witches. But for years, Huntington’s had this context of being associated with witchery, for whatever that's worth. It was unfortunate and it also was not true.
Robin Lindley: And the eugenics movement wanted to rid the US of Huntington’s disease—by sterilizing patients.
Dr. Thomas Bird: Yes. Because of the behavior of these people have and because of how abnormal they look and how deteriorated they get, Huntington’s got tossed into this pot of diseases we want to get rid of, especially because it was hereditary. So it got thrown into the eugenics movement in the first half of the 20th century. The eugenics movement in this country was focused at Cold Spring Harbor on Long Island. It's still a very prominent, biomedical research center even to this day. But back then, it was run by Charles Davenport, America's most prominent eugenicist. It's ironic that Cold Spring Harbor, Long Island, is only a few miles from East Hampton, Long Island, where Huntington lived.
Davenport's idea was that "bad diseases" are genetic. He said alcoholism is genetic. Mental illness is genetic. Mental retardation is genetic. Criminality is genetic. Prostitution is genetic. Dementia is genetic. And, Davenport said, we need to eliminate these from our society and we need to do it by sterilization. And he and the eugenics movement included Huntington's chorea as one of those diseases along with alcoholism and mental illness and criminality. So, Huntington's got a bad rap when it was thrown in with these diseases that were bad for the society, and they wanted to get rid of it by sterilizing people.
Robin Lindley: So eugenics was supposedly aimed at improving the health of the society, and there was also an element of class and racial discrimination.
Dr. Thomas Bird: Yes. And Huntington's became part of that. Being part of the eugenics theme and being part of the witch theme really gave Huntington's disease a very bad aura. It became a stigma for the communities. It became a stigma for the patients. It became a stigma for their families. So it was something they didn't want to face up to. Patients didn't want to talk about the kind of disease you'd hide in the closet. And it was really difficult to get a handle on this disease in the first half of the 20th century. Plus, because of their behavior and because of the fact that it hits you in your early and midlife, they'd lose employment and often become poverty stricken. They frequently ended up in mental institutions. So, it wasn't surprising that they got thrown into this pot of mental disease that we wanted to get rid of.
Robin Lindley: Was there evidence that the Nazis in Germany euthanized people with Huntington's as part of their T4 eugenics program, Hitler’s program to "eliminate" the disabled, those labeled as "life unworthy of life"?
Dr. Thomas Bird: I don't know if any of them were actually euthanized. I don't know if that's documented or not, but when you look at the lists of diseases that the Nazis wanted to get rid of, Huntington's clearly appears on those lists.
Robin Lindley: You mentioned too, and this touches on our regional history, that there tend to be more West Coast cases of Huntington's disease than in other parts of the country. Do you think that has something to do with migration patterns?
Dr. Thomas Bird: I think so. I can't argue too strongly for that because the statistics just aren't there. But when you go back and look at the population numbers for states (and this was mostly done by death certificates which aren't terribly accurate), there are certain states that were noted to have more families with Huntington's than others. If you look at those statistics HD seemed to be more prominent in Washington, Oregon and California.
When we started seeing families with Huntington's in the state of Washington, we wondered what was going on because we were seeing quite a few and we thought maybe they were all related. Maybe one family had moved to this area a hundred years ago, 120 years ago, and we were seeing the descendants of this one family. But we could look at the family trees of the families we were seeing and that clearly was not true. We were seeing very different families and hundreds of different families that were not related to each other. None of them were native western Washington people because there aren't very many native western Washington people. We're an area of migration, so it was clear that these families had come from the East and from Midwest.
We could see that the people with Huntington's that we saw were from families that had moved here from the East and the Midwest. When you looked at these death certificate reports, the Western states had a lot more Huntington’s than the Midwest states per population, so we thought that there was a migration factor and they were getting to the West Coast and couldn't go any farther, so they settled down.
Why would they migrate? In my mind, one of the reasons would be that people with Huntington's disease tend to be loners. They tend to want to go off by themselves. And they tend to be shunned by their communities because they look different, they act different, and they have social behavioral problems. They were not getting along in their local communities. So they moved. In our country when you move, more often than not, you move west. I think that's what happened to a certain degree.
Robin Lindley: That makes sense to me. I think Washington State has a reputation for attracting outcasts, misfits and loners. You also address the history of different approaches to treating Huntington's, including the use of lobotomy in the 20th century.
Dr. Thomas Bird: I didn't want to emphasize that very much, but it intrigued me because it became apparent to me that, particularly in the first half of the 20th century, it was common for people with Huntington's disease to get committed to state mental institutions. It's not so much now because there are fewer institutions and their populations have gone down but, up until the 1970s, it was very common for patients with Huntington's to be admitted to state mental institutions. And because they had a progressive disease that didn't get better, they tended to stay there for a long time, sometimes for the rest of their lives.
I ran into quite a few people with Huntington's disease in our state institutions and there was no good treatment for it then and there still isn't a good treatment for it. And, in the 1940s and 50s, Walter Freeman developed frontal lobotomy as a treatment for mental illness and it became extraordinarily popular. It was done mostly in mental institutions. Walter Freeman actually traveled around the country and showed psychiatrists and neurologists how to do frontal lobotomies. He went from state hospital to state hospital to state hospital doing that. And then [his trainees] would do it.
From 1938 to about the late 1960s, it was done on thousands of Americans in state institutions. I wondered, was it ever done on somebody with Huntington's disease? I actually had never seen anybody with Huntington's who had had that procedure, but it seemed to me, knowing they were in state institutions, knowing there was no good treatment for it, and knowing that this frontal lobotomy had become very popular in the fifties and sixties, the chances were that some people with Huntington's were getting lobotomies. I wondered if I could actually document such a case.
I went back to Walter Freeman's original textbooks on his procedure. He wrote two editions of his textbook and they [describe] the procedure. He [included] long lists of patients that he did the procedure on by number. He would give them a case number and then he'd just talk about them a little bit. I quickly realized that he didn't particularly use this procedure for certain kinds of mental illness. He thought lobotomy might be good for almost any mental illness, so he did it on all kinds of patients. He was doing it for schizophrenia and for depression. He was doing it on mania, he was doing it on dementia. In essence anybody that misbehaved he thought was a prime candidate for a frontal lobotomy.
I looked in his index of one of his volumes of his books to see if he listed Huntington's disease. And sure enough, he did. So, I found a case in his records of a patient with Huntington's disease that he had done a frontal lobotomy on. In my mind, that confirmed in fact that this was being done on people with Huntington's disease. I have no idea how many, but knowing that he saw nothing wrong with doing it on Huntington's and knowing that he showed hundreds of doctors how to do it, and knowing that it was fairly commonly done all over the country, my guess is that probably at least a hundred people with Huntington's had that procedure done and maybe even more.
Robin Lindley: And Freeman’s lobotomy was such a crude procedure that was done with an icepick and a hammer.
Dr. Thomas Bird: Yes. It was very crude and it was not controlled and it was not done in any careful scientific manner. And Freeman was an evangelist for it and he was self-promoting both himself and his procedure. It definitely was out of control. I don't want to emphasize it, but I think it is part of the story of what happened to people who had this disease.
Robin Lindley: And you discuss the role of the asylum movement in the history of Huntington’s.
Dr. Thomas Bird. Yes. Asylums were built for that kind of person. Actually, the asylum movement was a positive, compassionate approach to help the community and to help the patients with severe mental illness. If you look at the people who were promoting asylums in the 19th century, they were trying to help by doing two things. Number one, they were trying to treat these very sad people who were very difficult to help. They also were clearly trying to remove these people from society so that they would be separated out. They thought that made society safer and it made the patients safer. The problem was, once you put them away, nobody paid much attention to them. They could be abused and no one would know it. There was no mechanism for getting them back into society once they disappeared. And nobody wanted to pay a lot of money to take care of them.
And that of course is still a problem today. It's very expensive to take care of people in institutions. And by and large, the states and the communities don't want to put a lot of money into it. They complain bitterly about both the patients with these diseases and the institutions, but they don't want to fund them to a level that that will actually be effective.
Robin Lindley: Terrible problems developed with deinstitutionalization, by the 1970s, I believe, and many patients who were discharged from institutions wound up on the streets without support.
Dr. Thomas Bird: Yes. And Huntington's is one of many diseases where they commonly put patients into state institutions. And when the deinstitutionalization happened, they were put back out in the community, but nobody was paying much attention and they didn't really get the care that they ought to have. And today even, there are people with Huntington's who are homeless and are not getting good care because they seem to misbehave and they have no financial resources. They have what's called denial. They don't think there's anything wrong with themselves so they often refuse treatment and they refuse to take medications and they flounder in society.
Robin Lindley: The issue of lack of insight in the disease seems prominent.
Dr. Thomas Bird: It's very common. It was called denial, but they're not really consciously denying it. They really are not aware of their disability and lack of insight is a good way to put it. It’s lack of awareness. They're not aware of their behavioral abnormalities and they're not aware of their incoordination and involuntary movements, so they don't think they need help.
Robin Lindley: As your book demonstrates, you're a master storyteller. Can you tell me about your interest in writing and telling stories? Is it a matter of course for you as a physician to write about your cases?
Dr. Thomas Bird: I see patients in my mind. I see patients as human stories. I always talk to my patients. I always find out from my patients, who are they? What kind of work did they do? What was their occupation? Where did they live? Where were they born? Where did they go to school? Did they play sports? Did they have hobbies? Did they have any kind of talents? Who were their parents? Who were their brothers and sisters? What has their life been like? What got them to the office today? I always think of my patients that way. They're all human stories.
Robin Lindley: Did you keep case notes with those kinds of detailed descriptions?
Dr. Thomas Bird: In my clinic notes I always dictated the background of the patient. Where they were born, where they had lived, where they went to school, what their occupation was. I always thought that was part of their story and I thought of people that way.
And of course, the Huntington’s people would often have these problems with their occupations and with their marriages and with their families and with their behavior. They often were doing surprising things that you didn't expect and that would become part of their story. And sometimes they were recurrent and, month after month, I would see them and they were always having one problem after another. And some of them you couldn't forget because their problems were so complicated and sometimes so strange and sometimes so unusual and sometimes so difficult to deal with that you just couldn't forget them.
In fact, when I retired, I couldn't get these people out of my mind. I had seen dozens and dozens of them that I couldn't forget and I kept thinking about them. I thought one way to help me deal with that would be to get it down on paper. That's when I started writing their stories.
Robin Lindley: You vividly and compassionately describe your patients and share dozens of fascinating stories about them. You describe a man who had a compulsion to steal, and that seemed a part of his disease. He was in prison when he wrote you for help. Was his compulsion related to Huntington’s?
Dr. Thomas Bird: That individual’s story generated the name of my book. I got a totally unexpected letter in the mail. It was a handwritten letter and it began "Dr. Bird, Can you help me?" It turned out, as I read the letter, that it was from a prisoner in the state penitentiary in Walla Walla. He knew he had Huntington's chorea because his mother had died with it. He didn't say why he was in prison, but he asked if we had a clinic that followed people with Huntington's chorea. I wrote back to him and said that we did, and I just put it aside. I didn't think I'd ever hear from him again because I knew he was in prison and you don't go to the Walla Walla state penitentiary for minor crimes. I figured he would probably would be there for decades.
And then a few months later, he turned up in my clinic. I was actually a bit surprised. It turns out that the prison then was badly overcrowded and he had complained about having this disease, which was obvious because of his movements. The warden had told him that, if he could document that somebody would follow him for his disease on the outside, they would release him. So as soon as he got my letter, he showed it to the warden and they released him from prison on parole.
When he was out on parole, I saw him and followed him. I got a call one day from his parole officer who said he'd stolen a sweater from Nordstrom's. And the parole officer said,
“He's on parole and, if I report him for that, he'll go right back to prison.” And he said, “I like the guy and I don't want to send him back, and I know the pen is overcrowded anyway, so I'm going to let this go, but would you please tell him to stop stealing things?” And so, the next time I saw him, I did. I said, you know, don't do that or you'll end up back in jail. And he said he'd take that under consideration, but added that he couldn't help it. That was the way he put it. I think that's why he was in prison originally, because he had burglarized places over and over again.
A few months later, I got a call from the parole officer who said, “Sorry to tell you this, but he's back in the Walla Walla pen.” I asked, “Why?” And he said, “He burglarized a home, and the mistake he made was that he burglarized the home of a very wealthy, well known person.” It turned out to be the home of the owner of the famous Seattle restaurant, Rossellini's 410. And he was the brother of a former governor of the state. So it was a very prominent family. When they found out that the guy who had burglarized their house was on parole, they said he's got to go back. And so he did.
I talk in the book about whether his repetitive stealing had anything to do with his disease. That's sort of a leap. What's the proof that the two are related? Maybe he was just a burglar who happened to have Huntington's disease. But, if you look at the literature on Huntington's, it's very clear that one of the themes of the behavior problem can be obsessive compulsive illness. They can do things over and over again that they don't have any control over. They can become cigarette smokers. They can become alcoholics. They can become gamblers. They tend to be obsessive about a lot of things. Not always, but frequently. I think that's part of the disease. I suspect that this guy was a compulsive stealer because of his brain disease. I can't prove it, but I think it's very likely.
Robin Lindley: Doesn't this get into the neuroscience of addiction?
Dr. Thomas Bird: It gets into the organic brain foundation of mental illness. There’s this tendency to classify diseases as organic biologic diseases or mental diseases, and say they're not the same. If somebody has a mental illness, that's not like having cancer or diabetes. That's somehow different. But when you try and think that through, where does behavior come from? And that comes from their brain, right? It's not magic. Your language comes from your brain. Your vision comes from your brain. Your speech comes from your brain. Your walking, your talking, and your thinking come from your brain. So, doesn't mental illness, if we assume that there is mental illness, and I do, doesn't that come from your brain? And if you say that schizophrenia is a mental illness or manic-depressive or bipolar disease is a mental illness, doesn't that imply that it's a brain disease? So, if somebody is in a state institution or in a prison for abnormal behavior, how much of that is because their brains are not functioning properly, and is the right approach to that to just throw him in a cell and ignore him?
I think as a community we dropped the ball when we tried to deal with people with severe, difficult to control behavior. And I think we need to recognize at least some of that is being driven by abnormalities of the brain. Of course, environmental things are playing a role too. Your diet plays a role. Your parents play a role. Your peers play a role. Your occupation plays a role. Head trauma plays a role. All of those things are involved.
Robin Lindley: Are there a couple of other striking cases you'd like to mention?
Dr. Thomas Bird: I think people often don't realize that Huntington's has a juvenile piece. I have a case in the book that I call the "Princess in Pink" about this little girl who was in elementary school. She was a good student. She played soccer and kickball and she got along fine. She was just a really cute, nice kid. Then she started to have trouble. She couldn't run around as well anymore. And then she couldn't keep up with her peers in classwork, in reading and writing and arithmetic. She fell behind. And she was living with her grandmother because her mother died with Huntington's disease. Her family was aware of juvenile Huntington's, and they wondered, is that possible? Is our little girl developing juvenile Huntington's disease?
And it turned out to be exactly the case. When she was seven or eight years old, she actually began to deteriorate because she had developed this progressive disease. The nice thing about the story is that her teacher realized what was going on and she was particularly outgoing and kind to her and brought her classmates into her social welfare. And so, her classmates realized that she had a disease, that she was getting worse, but she was still this really nice girl that they'd known for several years already. And so, the teacher and the classmates formed this very effective safety net and support group for this little girl. And they wrote a class book about her called "Princess in Pink.” It's really a very compelling story.
Robin Lindley: You included much of the text of their lovely book for this girl, and it's very moving.
Dr. Thomas Bird: Yes, it was a lovely class project. . An awful lot of it had to do with the teacher who I have tremendous regard for, Ms. Perry. She stayed the girl's teacher for three years in a row. They developed a really good relationship and the students were really kind to the girl. She did very well for several years and stayed in school, but eventually became quite disabled and died with the disease, I think when she was 14. Her teacher and some of her students went to her funeral. So it's a sad disease, but it's a very nice story about what loving care she got from her social community.
Robin Lindley: That’s a touching chapter of your book. You also have the case of a man with Huntington’s who shot his roommate and he didn't know why.
Dr. Thomas Bird: I think that's another one of those lack of awareness kinds of things. He was just watching TV and he had a handgun and he pulled out the handgun and shot and killed his roommate and he didn't know why. He had Huntington's disease and he eventually went to prison.
And then I had the opposite case, where a man with Huntington's disease was killed by his roommate. That's a striking example of how vulnerable people with Huntington's are. I think he got in with the wrong crowd. He had no idea what a miserable guy he got attached to as a roommate. The roommate just decided to kill his friend who was obviously disabled with this disease. My guess is [the roommate] probably robbed him. So, on the one hand, a guy with Huntington's committed homicide, but on the other hand, a guy with Huntington's was very vulnerable and he was a victim of homicide. So, it can go either way.
So people with HD become very vulnerable. They can't take care of themselves and it's obvious to the community that there's something wrong with them either because of their behavior or their movements. And their judgment is very poor, so they can't figure out who's a good colleague and who's not a good colleague. And so, they often are abused by other people in the community because they're seen as disabled and vulnerable.
One of my favorite stories is about the young man who kept all his money in his shoe. He was homeless and he kept getting arrested. When he was in jail, he took the money out of his shoe and his cellmate noticed the money. His cellmate told him that he was a financial advisor and that, when they got out, if he turned his money over, he would invest it for him and make him a pile of money. And this guy with Huntington's was getting a VA pension, so he was getting monthly money. He met this "financial advisor" and started giving him all his money. He got the VA pension and of course his former cellmate was just stealing the money from it, and he ended up with nothing. Again, that shows how vulnerable he was.
Robin Lindley: You mention a tendency of Huntington patients to suffer head injuries.
Dr. Thomas Bird: Yes. I also have a picture in the book of an MRI of a person with a subdural hematoma. When they fall or hit their head, they bleed into the area between their brain and their skull. People with Huntington's are also vulnerable to mild head trauma and tend to get these subdural hematomas. There's a story in the book about a woman who fell down the stairs and she eventually died of subdural hematomas. We just recently had a man with HD who last month who died with subdural hematomas. Falls are bad news with this disease. It's a real problem.
We think what happens is that, with Huntington's, the brain tends to shrink from the degeneration so this space between the brain and the skull gets enlarged. There's more space there and that puts stress on the veins. And when a patient just hits his or her head against the wall or has what we would think of as mild trauma, the brain bleeds and there's a hemorrhage into the space between their skull and the brain. They're more vulnerable to that because their brain is shrinking.
Robin Lindley: Thanks for explaining that brain anomaly. I thought the head injuries were from movement problems and falling.
Dr. Thomas Bird: Yes, there is that. They hit the head more often because they are falling and bumping into things. But the kind of bump that wouldn't bother us can be very serious for them.
Robin Lindley: And there’s the vexing problem of suicide.
Dr. Thomas Bird:Yes. It's not so surprising, particularly for those who have awareness of their disease and especially if they've seen some other family member go through the full brunt of the disease. They don't want that to happen to them. So they can become very depressed and suicidal.
Robin Lindley: How can you treat or otherwise help these Huntington’s patients?
Dr. Thomas Bird: There are things you can do to help people and improve their lives. If you look at that context, the thing that helps the most is the helping community that you put around those people. If their families help them, their friends help them, their doctors help them, their nurses help them, their social workers help them, they do better. So what you need is a team that's focused on helping these people live their lives as best they can. And that's what helps them the most.
If they have certain symptoms, sometimes there are treatments for those symptoms. So if somebody is depressed, you can treat them with an antidepressant or you can do talk therapy and try to help them that way. There are some things that improve the movements. Some drugs slow down the movements. Of course, they have side effects, and sometimes it's a tradeoff. You slow down the movements, but you develop side effects. The same if they have delusions or, or psychotic behavior. There are drugs that are antipsychotics, and that sometimes improves that behavior. If they have severe anxiety, there are things that can improve anxiety.
So, there are things you can do to help people with Huntington's, but you don't cure the disease.
Getting back to it being a fatal disease, that brings up the issue of when it develops and the fact that it has this huge range of onset. It usually develops in the thirties or forties--those are the typical ages when you get it. And you may live for decades--three, four, five decades with no symptoms at all, and then develop the disease, and then live for 15 or 18 years. But there is a juvenile variety where children develop the disease. And there's a late onset variety where people don't develop it until they're in their seventies. So, if you develop it when you're 70 and 10 years later, you die of cancer, it wasn't really a fatal disease, right? So sometimes it is not as severe as it seems. As I say in my book, I've seen children who've had this disease when they were in an elementary school and I've also seen people who were in even their early nineties with the disease. The age range is surprisingly large.
Robin Lindley: You describe how the health care system often falls through for Huntington’s people and they don't get required care. What changes would you like to see with our health care system?
Dr. Thomas Bird: So, the people without financial and social resources need more help that they can't provide them themselves. If we really want to care for them compassionately, we've got to provide some resources for them. And that depends on what their problems are. If it's a medical problem, they need doctors and nurses and medication. If it's a social problem, they need housing, they need an occupation, they need social workers, they need appropriate diet. So, I think we need to put more resources into caring for people who, for no fault of their own, don't have those resources.
For people with progressive mental illness, particularly those that have lack of awareness, it's hard to care for them because they don't think there's anything wrong with them. But we have to be careful not to compromise their autonomy. People should be able to know in our country that they're free to behave in a wide range of ways as long as you don't hurt other people. But if you're injuring yourself or you're injuring people around you in some way, we have to try and get better care for you.
And if we can't put them in a state institution, then we need facilities in the community that are locally easily available that can care for them. And that's not easy if they don't want much care. But I think we need to provide as much as we can locally. For some people that means they need a controlled environment, at least for some period of time. It might be a week or a month or a couple of months, but there are some people that, for their own safety and health and for the safety and health of the community, need to be in a controlled environment for a while.
Robin Lindley: Wasn't the hope of those who advocated for deinstitutionalization that the mentally ill would have alternatives to institutions in their communities?
Dr. Thomas Bird: Unfortunately, too much emphasis was placed on saving money. What everybody saw with it was that deinstitutionalization would save money. They could close state hospitals or they could reduce their size and that would save millions of dollars. There was also this idea that new medications had been discovered that would so effectively treat these diseases that patients would not need close monitoring. You would just give them a pill and they would be fine. That idea turned out to be terribly naive.
Not enough resources were put into local facilities. There were some, but it wasn't anywhere near what was needed to really care for these people. And not only do you need a physical facility and not only do you need medications, but you need professionals who can care for patients and follow them and monitor them. That means doctors and nurses and medical staff and social workers who are trained and dedicated to care for these people who are difficult to care for. They're not simple. And so those professionals are expensive. The fact that you close down a state mental hospital doesn't mean that the adequate care of these people is going to be cheaper.
Robin Lindley: What are we learning from recent genetics research? Will it be possible in the future that some of the degenerative diseases like Huntington's disease can be prevented or somehow addressed with gene editing?
Dr. Thomas Bird: Yes. That's the hope right now. There's a very strong hope that the disease can be attacked from the genetic therapeutic standpoint and that there are ways to shut down the effects of the abnormal gene and basically turn it off. Whatever it's producing that's abnormal, you would stop and shut down and that would prevent the disease from progressing or from even developing. There's a lot of enthusiasm about doing that for Huntington's disease, and also all genetic diseases.
There have been a couple of successes in other diseases using that kind of approach. There's a disease of children called spinal muscular atrophy, a very severe condition. They've used a genetic approach to turn off that abnormal genetic mechanism and have the correct one work properly. It has been a huge benefit to these kids who otherwise would have died. There's a lot of enthusiasm for that.
And there is a study of Huntington's going on right now where they're using that kind of therapeutic approach and hoping that it will work. Probably in a year or two we'll know the results of that study. They're doing the same thing for genetic forms of ALS.
Robin Lindley: Is Alzheimer's in that category too?
Dr. Thomas Bird: Alzheimer's is more complicated because there are so many different causes of Alzheimer's and most Alzheimer's is not purely genetic. Huntington's is always purely genetic. Alzheimer's is usually not purely genetic, but there are some rare forms of Alzheimer's that are genetic diseases caused by a single mutation in a single gene. So in those rare kinds of Alzheimer's, that sort of approach is being considered.
Robin Lindley: Do you have any other comments for readers or anything to add about Huntington's or your research?
Dr. Thomas Bird: When I think back about Huntington's, the things I like to emphasize are that, for a medical science kind of person, it's a fascinating disease. It's also a tragic disease. And it's an important disease. Even though it's uncommon, I think it has important implications for all degenerative brain diseases and for mental illness. So I think its importance is way out of proportion to its uncommon frequency in the population. So it's fascinating. It's tragic. And it's important.
Robin Lindley: Thank you for your words Dr. Bird, and congratulations on your vivid and informative new book on Huntington's disease. Your compassion and devotion to your many patients with this perplexing and cruel condition is inspiring.